By Dr. Donald M . Voltz, MD, Autman Hospital,Ohio
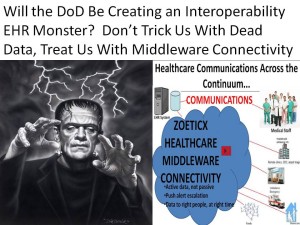 While many children will trick or treat, the DoD Healthcare Management System Modernization closes its bidding process today to replace their current EHR for active-duty personal and their families estimated at 11 billon taxpayer dollars. The current system, the Armed Forces Health Longitudinal Technology Application (AHLTA) will be replaced with a commercial system and the large amount of data migrated into the selected system. No question this is a huge decision and a complex health IT endeavor, both in the selection of an ideal solution to last for many years and the migration of a great deal of information from the legacy AHLTA to the newly selected EHR. The stakes are high for the vendors who threw their hat in the ring. This decision will lead to one of the largest migrations of health data from one system to another. The comprehensive AHLTA, implemented in 2004, supports nearly 10 million beneficiaries, storing their complete medical history, medically coded along with administrative information pertaining to their healthcare. Interestingly, AHLTA was the first EHR to have central storage of standardized patient health data with online access to all of this information, linking more than 450 treatment facilities around the world. However, with so much at stake, there are many concerns. The decision to rip and replace the AHLTA with any of the vendor systems bidding for this large contract raises as many questions as the decision attempts to address. This appears to violate the ONC’s requirements, whose guiding design principle clearly points out that any solutions must be built on top of an existing environment and avoid any disruption of service. How can the government violate its own guidelines? While the bidding process requires support of many health IT standards, these do not address the issue of usability of the data captured by the systems. As interoperability continues to plaque EHR systems, the big question here is one of information flow. Even if the data migration goes well, without interoperability, how will the DoD migrate participants and their families from active military to veteran status? Will DoD medical pros have access to the right data at the right time to provide the best medical outcomes for those who have sacrificed so much? It is absolutely essential for those bidding on the DoD to have a blueprint in place for the flow of information. This information flow is even more crucial for military members who might have been treated overseas, sent back to the US, and possibly sent home with outpatient care. Without the essential middleware-based connectivity “glue”, the backbone of interoperability proven successful in many industries, how will all of these disparate pieces of data be used in a meaningful way? Also, if the data is passive, not active and devoid of “push” technology to escalate attention to potential problems, we have the same old mess we have today, except it will be forced on additional millions of military members and their dependants! How we can solve these issues an provide DoD customers with the care they deserve. Despite A Decade of Innovation, Communications Still Lacking A great deal of innovation and evolution of EHR systems has taken place in the last decade, but much of this has been in the storage of data and the rest has been pieced together as regulations forced vendors to modify their platforms. The use of these systems for clinical care, especially as tools to enhance and promote communication between collaborative healthcare teams and the patients they are treating are still lacking. The system, at least for active-duty military personnel and their families, seems like it will wind up being the same interoperable one we are still struggling to implement for the general public and the current system itself is not all good news. Many claim the system is difficult to use. Military physicians spend most of their time working around system deficiencies rather than entering clinically relevant information, and data has been lost when the system is used by providers outside of military medical facilities. Not surprisingly, many of these same problems are reported with commercial EHR vendors and the basis for a major push to solve the problem of interoperability. Irrespective of the outcome from the bidding process, we are likely to learn a great deal about the migration of data between systems, but not likely to solve the challenges of interoperability between the selected EHR and EHRs used by outside providers taking care of our military. This initiative presents a great opportunity to look for another solution, one focused on connecting different EHR systems in a clinically manner. The previously mentioned issues of workflow and connectivity can be viewed as technical definitions, meaning different things to different people. At the clinical level, delivering healthcare in a safe, effective, timely and cost effective manner requires us to focus on the objective – Patient Medical Information Flow. Any solution that addresses this flow of information must become the blueprint for addressing EHR interoperability, something that is currently eluding us. Ill Defined Technical Problems of Interoperability and Information Flow A change in perspective from the ill-defined technical problem of interoperability to information flow is necessary to solve the challenges ahead for healthcare. Addressing the complexities with a single platform will continue to be a challenge as shown in many other industries. The history of medicine has similarities we can learn from to address the problems we have in health IT. Both have experienced internal and external pressures necessitating adapting in real-time to limit negative outcomes for patients, communities and society as a whole. We are beginning to appreciate that even with well defined technology standards, integrating all of the clinical, research, financial, population and administrative requirements into a single system that can respond to these changing pressures is unlikely. As we continue to work on standards, nomenclatures and taxonomies to better understand and manage the data being collected, we will need to look at other software technologic paradigms to address these challenges. The recently released ONC guiding design principles suggest solutions must be on top of existing systems so as to avoid disruption of service. The decision to migrate 10 million active-duty military personnel and their families to a new EHR platform will not be made in haste, especially with many comparing this to the healthcare.gov difficulties. The problem as I see it is with the overarching belief where all patient information must be consolidated and standardized in order to be shared and used for the management of patients and the effective delivery of care. Although current EHR technology has issues with providing the right information to the right person at the right time, they have done a fairly good job of collecting and organizing patient data. Building Customized Solutions on Top of EHRs Building customized solutions on top of these data models has the potential to address the usability and interoperability of data. Middleware software architecture has been shown to be an effective and efficient means to allow for customization while maintaining standardization and integrity of data. Given our current struggles and the competitive EHR landscape, could such a software design actually address these issues? Yes, given opening up access to the data. There appears to be a level of fear and loss of competitive advantage if vendors allow for outside development on their EHR platform. Granted there are token attempts for vendors to comply with regulations and address the requests of customers to expand the systems, complete open source does not exist with a few minor exceptions. Despite this limitation, successful implementation of a middleware architecture has been developed to connect different EHR systems, interact with the data contained in the systems and display it in a uniform and clinically relevant manner. Zoeticx has developed such a middleware platform and demonstrated its ability to connect to EHR systems including VistaA and AllScripts. The platform has developed the necessary framework to connect to other systems as well using API’s and tools provided by vendors, even if they are not completely open with the underlying code. From a clinical standpoint, as long as data integrity, security and providence are maintained, it does not matter where the information I am viewing resides, my patient comes from. As a patient moves from one office to another or is transferred from one hospital for definitive management at another, the view into the data does not need to include the vendor EHR or comply with their choice of design and display. In addition, as I use the data to make decisions, this is captured by whatever system the patient is currently registered under. Reconstructing the flow of information, from what system it originated and how it impacted care at another, can be captured bringing more meaning to the individual care and providing the ability to manage population management at larger system levels. Instead of creating a pieced together monster brought to life with a lightning bolt, we need to build a system that is responsive to changing environmental pressures and can adapt to meet the needs of all stakeholders and address the underlying problem – Patient Medical Information Flow.
While many children will trick or treat, the DoD Healthcare Management System Modernization closes its bidding process today to replace their current EHR for active-duty personal and their families estimated at 11 billon taxpayer dollars. The current system, the Armed Forces Health Longitudinal Technology Application (AHLTA) will be replaced with a commercial system and the large amount of data migrated into the selected system. No question this is a huge decision and a complex health IT endeavor, both in the selection of an ideal solution to last for many years and the migration of a great deal of information from the legacy AHLTA to the newly selected EHR. The stakes are high for the vendors who threw their hat in the ring. This decision will lead to one of the largest migrations of health data from one system to another. The comprehensive AHLTA, implemented in 2004, supports nearly 10 million beneficiaries, storing their complete medical history, medically coded along with administrative information pertaining to their healthcare. Interestingly, AHLTA was the first EHR to have central storage of standardized patient health data with online access to all of this information, linking more than 450 treatment facilities around the world. However, with so much at stake, there are many concerns. The decision to rip and replace the AHLTA with any of the vendor systems bidding for this large contract raises as many questions as the decision attempts to address. This appears to violate the ONC’s requirements, whose guiding design principle clearly points out that any solutions must be built on top of an existing environment and avoid any disruption of service. How can the government violate its own guidelines? While the bidding process requires support of many health IT standards, these do not address the issue of usability of the data captured by the systems. As interoperability continues to plaque EHR systems, the big question here is one of information flow. Even if the data migration goes well, without interoperability, how will the DoD migrate participants and their families from active military to veteran status? Will DoD medical pros have access to the right data at the right time to provide the best medical outcomes for those who have sacrificed so much? It is absolutely essential for those bidding on the DoD to have a blueprint in place for the flow of information. This information flow is even more crucial for military members who might have been treated overseas, sent back to the US, and possibly sent home with outpatient care. Without the essential middleware-based connectivity “glue”, the backbone of interoperability proven successful in many industries, how will all of these disparate pieces of data be used in a meaningful way? Also, if the data is passive, not active and devoid of “push” technology to escalate attention to potential problems, we have the same old mess we have today, except it will be forced on additional millions of military members and their dependants! How we can solve these issues an provide DoD customers with the care they deserve. Despite A Decade of Innovation, Communications Still Lacking A great deal of innovation and evolution of EHR systems has taken place in the last decade, but much of this has been in the storage of data and the rest has been pieced together as regulations forced vendors to modify their platforms. The use of these systems for clinical care, especially as tools to enhance and promote communication between collaborative healthcare teams and the patients they are treating are still lacking. The system, at least for active-duty military personnel and their families, seems like it will wind up being the same interoperable one we are still struggling to implement for the general public and the current system itself is not all good news. Many claim the system is difficult to use. Military physicians spend most of their time working around system deficiencies rather than entering clinically relevant information, and data has been lost when the system is used by providers outside of military medical facilities. Not surprisingly, many of these same problems are reported with commercial EHR vendors and the basis for a major push to solve the problem of interoperability. Irrespective of the outcome from the bidding process, we are likely to learn a great deal about the migration of data between systems, but not likely to solve the challenges of interoperability between the selected EHR and EHRs used by outside providers taking care of our military. This initiative presents a great opportunity to look for another solution, one focused on connecting different EHR systems in a clinically manner. The previously mentioned issues of workflow and connectivity can be viewed as technical definitions, meaning different things to different people. At the clinical level, delivering healthcare in a safe, effective, timely and cost effective manner requires us to focus on the objective – Patient Medical Information Flow. Any solution that addresses this flow of information must become the blueprint for addressing EHR interoperability, something that is currently eluding us. Ill Defined Technical Problems of Interoperability and Information Flow A change in perspective from the ill-defined technical problem of interoperability to information flow is necessary to solve the challenges ahead for healthcare. Addressing the complexities with a single platform will continue to be a challenge as shown in many other industries. The history of medicine has similarities we can learn from to address the problems we have in health IT. Both have experienced internal and external pressures necessitating adapting in real-time to limit negative outcomes for patients, communities and society as a whole. We are beginning to appreciate that even with well defined technology standards, integrating all of the clinical, research, financial, population and administrative requirements into a single system that can respond to these changing pressures is unlikely. As we continue to work on standards, nomenclatures and taxonomies to better understand and manage the data being collected, we will need to look at other software technologic paradigms to address these challenges. The recently released ONC guiding design principles suggest solutions must be on top of existing systems so as to avoid disruption of service. The decision to migrate 10 million active-duty military personnel and their families to a new EHR platform will not be made in haste, especially with many comparing this to the healthcare.gov difficulties. The problem as I see it is with the overarching belief where all patient information must be consolidated and standardized in order to be shared and used for the management of patients and the effective delivery of care. Although current EHR technology has issues with providing the right information to the right person at the right time, they have done a fairly good job of collecting and organizing patient data. Building Customized Solutions on Top of EHRs Building customized solutions on top of these data models has the potential to address the usability and interoperability of data. Middleware software architecture has been shown to be an effective and efficient means to allow for customization while maintaining standardization and integrity of data. Given our current struggles and the competitive EHR landscape, could such a software design actually address these issues? Yes, given opening up access to the data. There appears to be a level of fear and loss of competitive advantage if vendors allow for outside development on their EHR platform. Granted there are token attempts for vendors to comply with regulations and address the requests of customers to expand the systems, complete open source does not exist with a few minor exceptions. Despite this limitation, successful implementation of a middleware architecture has been developed to connect different EHR systems, interact with the data contained in the systems and display it in a uniform and clinically relevant manner. Zoeticx has developed such a middleware platform and demonstrated its ability to connect to EHR systems including VistaA and AllScripts. The platform has developed the necessary framework to connect to other systems as well using API’s and tools provided by vendors, even if they are not completely open with the underlying code. From a clinical standpoint, as long as data integrity, security and providence are maintained, it does not matter where the information I am viewing resides, my patient comes from. As a patient moves from one office to another or is transferred from one hospital for definitive management at another, the view into the data does not need to include the vendor EHR or comply with their choice of design and display. In addition, as I use the data to make decisions, this is captured by whatever system the patient is currently registered under. Reconstructing the flow of information, from what system it originated and how it impacted care at another, can be captured bringing more meaning to the individual care and providing the ability to manage population management at larger system levels. Instead of creating a pieced together monster brought to life with a lightning bolt, we need to build a system that is responsive to changing environmental pressures and can adapt to meet the needs of all stakeholders and address the underlying problem – Patient Medical Information Flow.

